Obsessive-Compulsive Disorder (OCD) has intrigued and challenged humanity for centuries. This deep dive into OCD’s evolution reveals how perceptions and treatments have transformed from ancient superstitions to cutting-edge science.
From ancient beliefs to modern science, the understanding and treatment of OCD have evolved considerably. Our journey begins in ancient civilizations, where OCD-like symptoms were often attributed to supernatural forces or a lack of moral character. Consider ancient Egypt, where mental disorders were often attributed to evil spirits, reflecting the era’s spiritual interpretation of mental health.
Fast forward to the Middle Ages, and OCD was perceived as a form of madness, leading to stigmatization and marginalization. However, in the 19th and 20th centuries, significant advancements in psychology and medical science shed new light on OCD.
The work of prominent figures like Sigmund Freud and Ivan Pavlov paved the way for a deeper understanding of the disorder’s psychological and physiological aspects. Today, thanks to modern science, we have a more comprehensive understanding of OCD as a neurobiological condition.
In the 21st century, our understanding of OCD has expanded dramatically. Recent studies indicate that OCD affects approximately 1-2% of the population globally, with emerging treatments like Transcranial Magnetic Stimulation (TMS) showing promise. This shift from historical misconceptions to evidence-based approaches marks a significant milestone in mental health care.
Research has revealed intricate brain mechanisms and led to the development of evidence-based treatments, offering hope and relief for those affected by this debilitating disorder. In this comprehensive guide, we get into the roots of OCD, exploring its evolution, subtypes, and the often-overlooked connection between OCD and addiction.
From supernatural explanations to cultural interpretations, understanding how OCD was perceived in ancient times provides valuable insights into the evolution of our comprehension.
In ancient civilizations, mental disorders, including symptoms resembling OCD, were often attributed to supernatural forces. In ancient Egypt, for instance, religious beliefs connected such conditions to the influence of evil spirits. This perspective framed mental health challenges as divine punishments.
Another prevailing misconception was the idea that individuals with symptoms resembling OCD lacked moral character. The Middle Ages saw OCD being perceived as a form of madness, leading to stigmatization and marginalization. This belief placed the blame on the person’s character rather than understanding it as a complex mental condition.
Some ancient cultures viewed mental disorders, including what we now recognize as OCD, as a form of punishment for wrongdoings. This perspective reinforced societal judgments and often hindered individuals from seeking the help they needed.
The absence of scientific understanding in ancient times contributed to misconceptions about the nature of OCD. Without the knowledge we have today, explanations were often rooted in cultural beliefs and superstitions.
These ancient beliefs had significant implications for individuals dealing with OCD-like symptoms. Instead of seeking understanding and support, they faced judgment, isolation, and sometimes even harsh treatment based on these misconceptions.
As we journey through time, it becomes evident that the understanding of OCD has evolved. Prominent figures in psychology and medicine, such as Sigmund Freud and Ivan Pavlov, played crucial roles in shifting the narrative. Their work laid the foundation for a more nuanced understanding of OCD as a complex neurobiological condition.
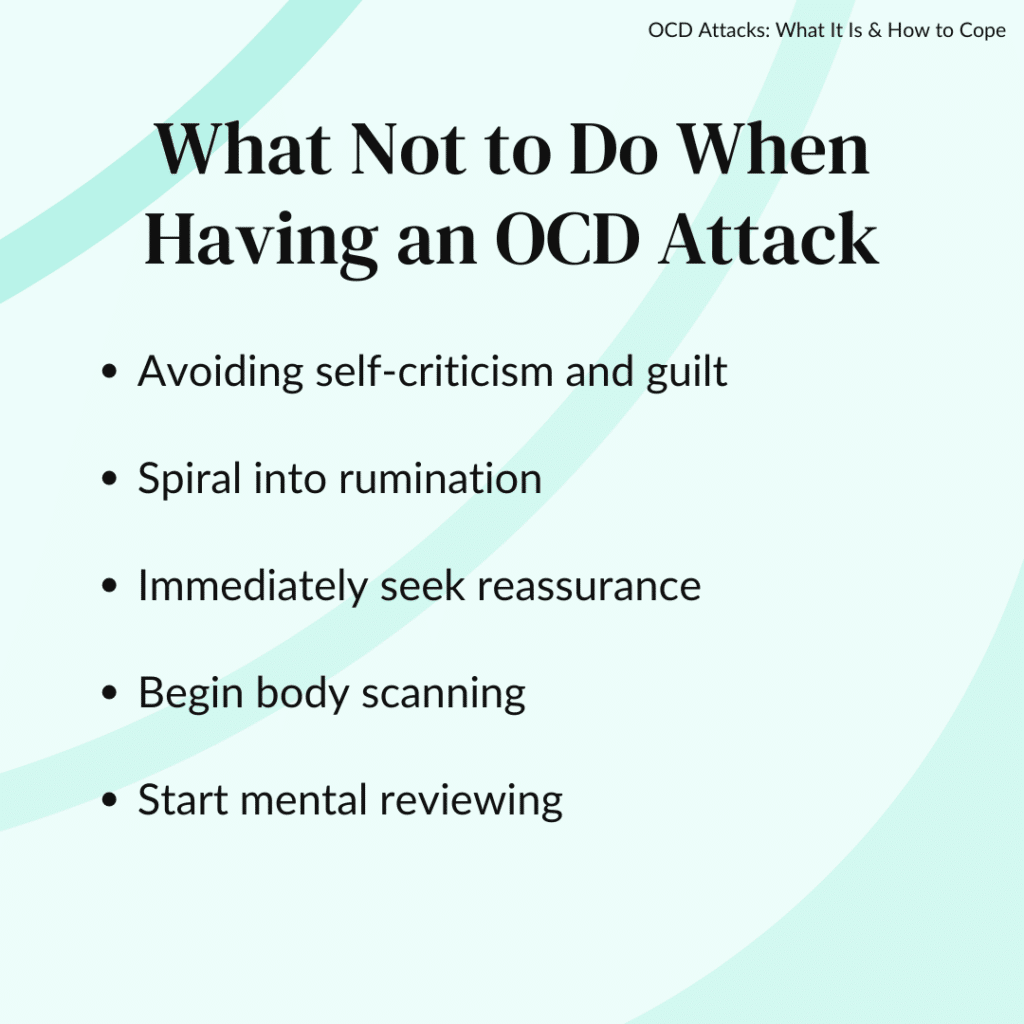
Obsessive-Compulsive Disorder (OCD) can sometimes lead to something called an “OCD attack.” It’s like a tough moment that some people with OCD go through. Let’s break down what that means.
An OCD attack is when someone with OCD has a period of intense feelings and thoughts that can be really overwhelming. During these times, their mind gets filled with thoughts that are hard to control. These thoughts are called “obsessions.”
Imagine if your brain kept telling you that something bad might happen, or you need to do something a certain way to keep things safe. These thoughts can make someone feel very anxious and worried.
To deal with these thoughts, a person might do certain things over and over again. These actions are called “compulsions.” It’s like a way for them to feel a bit better, even if it’s just for a little while.
Obsessive-Compulsive Disorder (OCD) and addiction, seemingly disparate in nature, reveal a complex relationship that has garnered significant attention in the realms of psychology and psychiatry. Unraveling the intricacies of this interplay involves a deep exploration of how these conditions coexist, influence each other, and shape the experiences of individuals.
This discussion aims to shed light on the nuanced connections, historical perspectives, and contemporary insights into the intricate relationship between OCD and addiction.
Obsessive-Compulsive Disorder (OCD) is a mental health condition that manifests in various ways, and understanding its subtypes is crucial for a comprehensive grasp of the disorder. Subtypes of OCD refer to distinct categories of obsessive thoughts and compulsive behaviors that individuals may experience. Exploring these subtypes sheds light on the diversity and complexity of OCD presentations, moving beyond the stereotypical portrayals often seen in media.
Understanding the subtypes of OCD provides a nuanced perspective on the disorder, recognizing the unique challenges faced by individuals across different categories. This awareness is vital for clinicians, researchers, and the general public, fostering empathy and informed support for those navigating the complexities of Obsessive-Compulsive Disorder.
The exact cause of OCD attacks is unknown, but there are several factors that may contribute to their development. These include:
Imagine being in a really stressful situation. For someone with OCD, this stress can act as a spark that sets off an OCD attack. It’s like their brain goes into overdrive with obsessive thoughts.
Big changes in life, like moving to a new place, starting a new job, or going through a major life event, can be a trigger. These changes can make the brain kick into high gear with worries and compulsions.
Sometimes, unexpected things happen that catch us off guard. For someone with OCD, these unexpected events can become a trigger, making their thoughts and rituals more intense.
Strong emotions, whether it’s sadness, anger, or fear, can act as a trigger. When emotions run high, OCD thoughts and compulsions may become more pronounced.
Each person with OCD might have specific things that set off their attacks. It could be certain objects, situations, or even specific numbers. These personal triggers are unique to each individual.
A strong inclination towards perfectionism, where individuals set unrealistically high standards for themselves, can act as a trigger for OCD attacks. The constant pursuit of flawlessness and the fear of making mistakes may intensify obsessive thoughts and compulsive behaviors.
Peer pressure or societal expectations can contribute to the development of OCD attacks. The need to conform to perceived norms or fear of judgment may amplify the anxiety and rituals associated with obsessive-compulsive tendencies. Social factors can play a significant role, especially in individuals prone to external validation.
Understanding the causes of OCD attacks is a complex process, and it’s often a combination of these factors that contributes to the development of obsessive-compulsive symptoms. While pinpointing a single cause remains challenging, recognizing these triggers can be a crucial step toward managing and treating OCD effectively.
When someone is going through an OCD attack, it can make daily life more challenging. They might spend a lot of time doing these repetitive actions, which can get in the way of doing things they enjoy or need to get done. It’s like having a big mental struggle that can be exhausting.
Imagine having a routine, but now add some extra steps that you feel you must do. For someone with OCD, daily rituals or compulsions can take up a lot of time. It might be washing hands repeatedly or checking things over and over.
Daily tasks like getting ready, going out, or even working can get interrupted by obsessive thoughts. These thoughts can make someone feel like they have to stop everything and address their worries.
OCD can bring a constant sense of anxiety. It’s like having a worry cloud hanging over you all the time. This anxiety can make it challenging to relax or enjoy activities.
Making decisions, even small ones, can become a big challenge. OCD might make someone doubt their choices, leading to a cycle of overthinking.
OCD can affect how someone interacts with others. They might need reassurance or have specific ways of doing things that others might not understand. This can sometimes strain relationships.
Dealing with the constant thoughts and rituals can be draining. It’s like running a mental marathon every day, leaving a person feeling mentally and physically exhausted.
The modern understanding of Obsessive-Compulsive Disorder (OCD) has undergone a profound transformation, shaped by scientific advancements, psychological insights, and a growing awareness of mental health. Here are some of the key milestones that mark the emergence of our contemporary understanding of OCD.
The late 19th and early 20th centuries saw the emergence of influential figures in psychology, notably Sigmund Freud. Freud’s exploration of the unconscious mind and his acknowledgment of the psychological aspects of mental health laid the groundwork for understanding conditions like OCD.
Ivan Pavlov’s groundbreaking work on classical conditioning further contributed to the modern understanding of OCD. The exploration of learned behaviors and responses paved the way for recognizing the behavioral aspects of obsessive-compulsive symptoms.
The mid-20th century witnessed significant strides in neuroscience, allowing researchers to delve into the intricate workings of the brain. Modern imaging techniques and studies on brain chemistry provided insights into the neurobiological underpinnings of OCD, elevating it from a purely psychological understanding.
The inclusion of OCD in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) in 1980 marked a pivotal moment. This official recognition solidified OCD as a distinct mental health disorder, prompting increased research and public awareness.
The development and widespread acceptance of Cognitive-Behavioral Therapy (CBT) revolutionized the treatment landscape for OCD. CBT, particularly exposure and response prevention, became a gold standard in helping individuals manage and overcome obsessive-compulsive symptoms.
The identification of serotonin reuptake inhibitors (SSRIs) as effective medications for OCD provided another dimension to its treatment. Medications, when combined with therapy, offered comprehensive support for individuals dealing with OCD.
The latter part of the 20th century and the early 21st century witnessed a growing global awareness and advocacy for mental health. Organizations and individuals worldwide have played a crucial role in reducing stigma, fostering understanding, and promoting access to mental health resources.
1. Global Prevalence: According to the World Health Organization, OCD is among the top 20 causes of illness-related disability for individuals aged 15-44.
2. Onset and Duration: Typically begins in childhood or early adulthood, with symptoms often persisting throughout life.
3. Anxiety Connection: Anxiety is a core element of OCD, triggered by persistent, intrusive thoughts.
4. Diverse Symptoms: OCD presents in various forms, with obsessions ranging from contamination fears to concerns about harm, and compulsions involving rituals like counting or checking.
5. Neurobiological Basis: Imbalances in neurotransmitters and structural/functional brain abnormalities contribute to the neurobiological underpinnings of OCD.
6. Treatment Efficacy:
Research shows that up to 70% of patients with OCD benefit from either medication or Exposure and Response Prevention (ERP) therapy.
7. Economic Impact:
OCD costs the U.S. economy billions annually in lost earnings and healthcare expenses.
The journey to understand and treat Obsessive-Compulsive Disorder (OCD) is an ongoing and dynamic exploration, marked by remarkable progress and promising advancements. The field has witnessed significant strides in unraveling the intricate neurobiological underpinnings of OCD, leading to more targeted and effective treatment strategies.
Neuroscientific breakthroughs, including advancements in imaging technologies and neurotransmitter research, have provided unprecedented insights into the neural pathways involved in OCD. This deeper understanding has paved the way for innovative therapeutic approaches, such as enhanced Cognitive-Behavioral Therapy (CBT), Deep Brain Stimulation (DBS), and the exploration of glutamate modulators and cannabinoids.
The integration of digital therapeutics, including mobile applications and online platforms, represents a contemporary frontier in OCD treatment. These tools offer accessible and supplementary avenues for individuals to engage in self-help strategies, monitor symptoms, and receive ongoing support.
As the journey unfolds, it is clear that the traditional boundaries of OCD treatment are expanding. The emergence of novel interventions and the refinement of existing approaches underscore a commitment to providing more personalized, effective, and holistic care for individuals grappling with OCD.
This ongoing pursuit reflects not only the dedication of researchers and clinicians but also the resilience and strength of individuals facing the challenges posed by Obsessive-Compulsive Disorder.
Looking ahead, the collaborative efforts of the scientific community, coupled with the courage and advocacy of those impacted by OCD, will continue to shape the landscape of understanding and treatment. Our journey through OCD’s history underscores a future of hope and empowerment. As we continue to unravel the complexities of OCD, we pave the way for more personalized, effective treatments, ensuring that those affected can lead fulfilling lives.