Do you feel empty and like there’s nothing left in life? Are you facing sadness, anxiety, fatigue, harmful thoughts, and helplessness now and then which is just never-ending? There’s a possibility that you are suffering from depression, the phase of your life when everything is a mess for you and you feel like nothing can be fixed. This can be so tough that words can fall short of describing what you are undergoing. Get to know about what causes depression in brain.
If not treated, it can adversely affect you and the people around you. It might have already affected your life. But before seeking help, it is essential to be aware of the causes of depression and how to identify these causes.
It is often said that before you find the cure, it’s always important to know the cause of a problem to ensure that you fix the problem from the root.
Well, this applies to depression too!
This ultimate guide will significantly help you to know what causes depression in the brain. Once you understand how to identify the causes of depression you can get proper help with suitable depression treatment.
So, let’s jump in!
What Exactly Is Depression?
Some people often confuse depression with the mood fluctuations that they regularly experience as a part of life.
Mood swings and everyday feelings are different from depression. Life can be affected by depression in many ways, including interactions with family, friends, and the community at large.
In simple terms, it is a mood disorder that can persist for a short or long period.
This disorder causes enduring feelings of sadness, sorrow, emptiness, and constant loss of joy. There can be certain events in one’s life that can trigger depression. (For example, loss of a loved one or loss of job)
According to the American Psychiatric Association, a common and serious disease, depression is a mental illness that affects how you feel, how you think, and how you act.
It also states that depression can cause feelings of sadness and/or a loss of interest in activities you once enjoyed. As a result, a depressed person can face a variety of emotional and physical problems causing a decrease in his or her ability to function at work and home.
In the United States, an estimated 21.0 million adults experienced at least one major depressive episode in 2021.
How Is Depression Different From Grief?
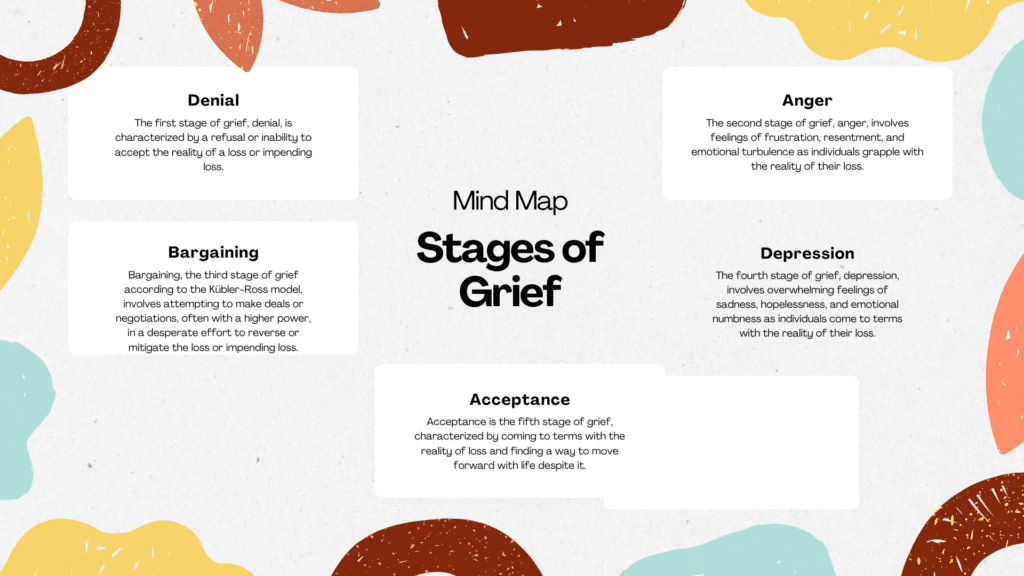
Although grief and depression may both contain sadness, they are distinct from each other.
Depression is a serious medical illness that significantly and negatively affects the daily aspects of your life. Grief is how you cope with a loss in your life such as a divorce, loss of home, or loss of a loved one.
Let’s have a closer look at the key differences between both.
Key Differences Between Depression And Grief
- The primary difference is that grief is regarded as an overwhelming emotional response to a loss, while depression is considered a serious mental health disorder that must be treated.
- Both experiences can have different origins or causes. Loss is a direct cause of grief. A significant loss may occasionally be a component of depression, but there are often other complex contributing elements as well, including problems with mood regulation in the brain, stressful life circumstances, genetics, or trauma.
- Depression can get worse and persist if proper treatment is not done, while grief frequently doesn’t require professional care.
- Depression symptoms can affect all aspects of your life and tend to linger longer, but symptoms of grief last shorter and tend to lessen over time.
- Grief might come in waves, especially after a few days. Some days you might be able to appreciate and feel pleasure, such as when you catch yourself laughing with friends while you think about a loved one who has passed away, while the next you might feel absolutely hopeless and joyless.
- Although symptoms of depression can emerge in waves as well, they are typically more powerful, persistent, and present every day for two or more weeks. When neglected, symptoms frequently get worse and have a big impact on your life.
Besides the above differences, depression and grief can also appear and feel alike in many ways. For a better understanding, we have listed some of their similarities below.
Key Similarities Between Depression And Grief
- Depression and grief can both cause sadness and sorrow. When you are grieving or depressed, you could find yourself sobbing a lot, getting cranky, and going through a lot of emotional suffering.
- Both depression and grief can affect your eating habits resulting in poor appetite.
- Your sleeping patterns may also change as a result of depression and grief. For instance, you might discover that you don’t want to do anything or struggle to get out of bed.
- Also, both grief and depression may be accompanied by angry outbursts.
The role of brain chemistry in depression
Our brains are incredibly complex organs, consisting of billions of nerve cells called neurons that communicate with each other through chemical messengers known as neurotransmitters. These neurotransmitters play a crucial role in regulating our mood, emotions, and overall mental well-being.
When imbalances occur in these neurotransmitters, it can disrupt the brain’s delicate equilibrium, leading to a range of mental health disorders, including depression. Serotonin, dopamine, and norepinephrine are among the key neurotransmitters that play a significant role in mood regulation.
Brain Areas Involved With Depression
According to Harvard Health Publishing, three prominent areas of the brain are mainly involved with depression. Let’s try to understand more about these areas below.
-
Amygdala
The amygdala is a component of a network of deep brain regions that are linked to feelings including anger, pleasure, sorrow, fear, and sexual arousal. The amygdala becomes active when a memory with strong emotional content, such as a terrifying experience, is recalled.
When a person feels sad or clinically depressed, their amygdala is more active, and this remains the case long after they have recovered from their depression. The amygdala may actually grow larger as a result of this increase in activity.
-
Basal Ganglia
The basal ganglia are a family of interconnected brain regions. They connect to and communicate with areas of the brain that are closer to the surface. They might aid in facilitating movement and take part in thinking, remembering, and emotional processing.
In some studies, it was found that people with depression had their basal ganglia shrink and other structural changes.
-
Hippocampus
The processing of long-term memory is significantly influenced by the hippocampus. It plays an important part in memory and learning.
For instance, this area of the brain detects fear when you are approached by a harmful animal, and the memory of such an encounter may cause you to be cautious around it in the future.
Some depressed individuals have a smaller hippocampus, and research implies that persistent stress hormone exposure stunts the neuronal growth in this region of the brain.
Neurotransmitters and their impact on mood
Imbalances in serotonin: The happiness hormone
Serotonin, often referred to as the “happiness hormone,” is responsible for regulating mood, sleep, and appetite. Low levels of serotonin have been linked to depression, as it can lead to feelings of sadness, irritability, and a general sense of unease.
Several factors can contribute to imbalances in serotonin levels. Genetic predisposition, stress, and certain medications or substances can all impact the production and function of serotonin in the brain. Understanding these factors can help healthcare professionals develop targeted treatments to restore balance and alleviate symptoms of depression.
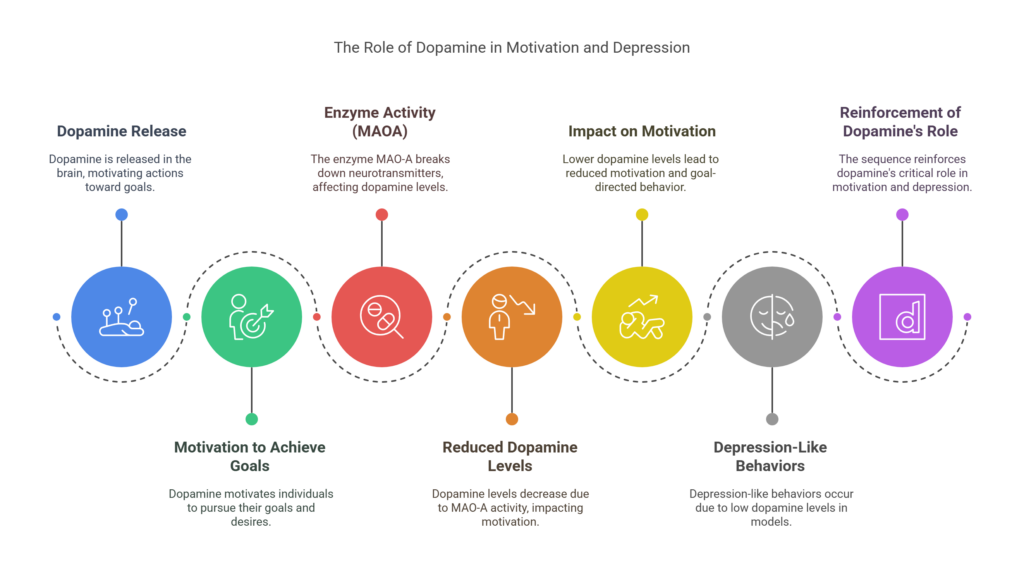
The role of dopamine in motivation and pleasure
Dopamine is a neurotransmitter associated with pleasure, motivation, and reward. It plays a crucial role in our ability to experience joy and feel motivated to engage in activities that bring us happiness. Imbalances in dopamine levels can severely impact mood and contribute to symptoms of depression.
Individuals with low levels of dopamine may experience a lack of interest or pleasure in activities they once enjoyed. They may also struggle with motivation and find it challenging to set and achieve goals. Understanding the role of dopamine in depression can inform treatment approaches that focus on restoring dopamine balance and enhancing the individual’s capacity for pleasure and motivation.
Norepinephrine and its effect on energy and focus
Norepinephrine is a neurotransmitter that helps regulate energy levels, attention, and focus. Imbalances in norepinephrine can lead to symptoms such as fatigue, lack of concentration, and difficulty staying motivated. These symptoms are often prominent in individuals with depression.
Understanding the impact of norepinephrine imbalances on mood and cognition can guide treatment strategies that aim to restore energy and improve focus. Medications that target norepinephrine reuptake or enhance its function can be effective in alleviating symptoms and promoting a more balanced mental state.
The impact of imbalances in GABA and glutamate
While serotonin, dopamine, and norepinephrine often steal the spotlight when discussing depression, imbalances in other neurotransmitters such as gamma-aminobutyric acid (GABA) and glutamate can also contribute to the development and progression of the illness.
GABA is an inhibitory neurotransmitter that helps regulate anxiety and stress. Imbalances in GABA levels can lead to increased anxiety and contribute to depressive symptoms. On the other hand, glutamate is an excitatory neurotransmitter that plays a role in learning and memory. Dysregulation of glutamate can disrupt neural circuits involved in mood regulation and contribute to depression.
Understanding the intricate interplay between these neurotransmitters and their impact on mood can provide valuable insights into the complex nature of depression. By targeting these imbalances, healthcare professionals can develop more personalized and effective treatment strategies.
Is There A Way To Identify The Cause Of Depression In The Brain?
Realizing that depression is a mental disorder that can be treated is essential at the fundamental level. Identifying the cause of your depression is equally important to get proper treatment.
One of the most reliable ways to identify the cause of depression is by talking about your problem to someone who can help you. Talking is considered one of the best therapies for coping with depression.
You can try to talk about it to someone close to you if possible, if not seek medical help from from therapists.
The process will help in identifying the exact cause of depression that you are facing. This will facilitate diagnosing depression and getting suitable treatments further.
Apart from identifying the causes, knowing the common symptoms of depression can also help a lot in diagnosing it. Below are some early signs of depression.
Early Signs Of Depression
- Unpredictable mood swings
- Restlessness
- Anxiety
- Irritability
- Loss of interest in activities
- Anger and aggression
- Thoughts of self-harm
Physical Impacts
- Back pain
- Gastrointestinal problem
- Fatigue and headaches
- Chronic joint pain
- Tiredness
- Loss Of Appetite
- Insomnia
What Causes Depression In The Brain?
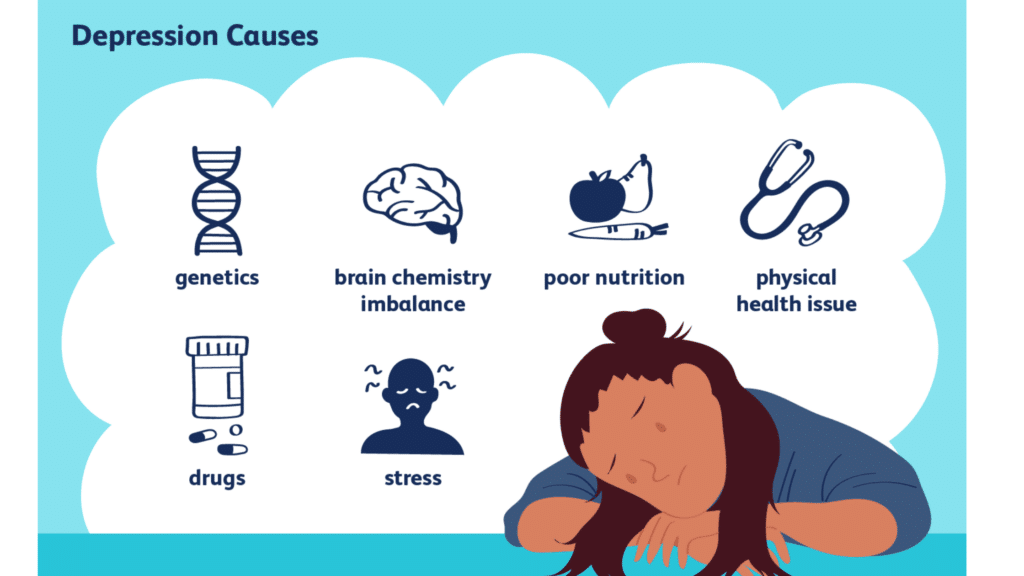
Although it’s frequently said that depression is caused by a chemical imbalance, this figure of speech fails to convey how intricate the condition is.
A certain brain chemical that is too much or too little does not necessarily cause depression, is what research says. Instead, there are other likely causes for depression, such as faulty mood regulation by the brain, hereditary susceptibility, and traumatic life experiences.
Actually, it is believed that a number of these factors combine to cause depression. Let’s dive deep and try to understand more about the causes of depression.
1. Inherited Traits
Some people can have a higher genetic risk for depression because it can run in families.
It is more common in people whose blood relatives also have this condition. In comparison to the average person, someone who has a parent or sibling with serious depression is likely to have a 2–3 times higher chance (20–30% instead of 10%) of undergoing depression.
However, you won’t necessarily experience depression if your parent or another close relative does. Even so, it’s likely that personal characteristics and circumstances will also play a significant role.
2. Drug Abuse And Alcohol Addiction
People who are struggling with drug abuse or alcohol addiction are frequently depressed. This can cause or exacerbate depressive symptoms like loneliness, despair, and hopelessness.
Drug abuse can alter the structure and functioning of the brain, increasing the risk of developing mental health issues including depression. Dopamine levels are known to be lower in depressed individuals, and the abuse of drugs can even worsen these levels.
When you drink alcohol, your inhibition-controlling part of the brain may work better, so you may feel more relaxed, less anxious, and more confident afterward. But these effects quickly wear off. The chemical changes in your brain can soon lead to more negative feelings, such as anger, anxiety, and ultimately depression, regardless of your mood.
3. Childhood Trauma
A person is more likely to subsequently experience depression and drug addiction if they had experienced trauma as a child. The loss of a parent, sexual or psychological abuse, domestic violence, and neglect are a few examples of situations that can trigger childhood trauma and stress in a person.
According to clinical studies, stress during childhood lowers levels of the “feel-good hormone” oxytocin, which has an impact on relationships and sentiments of trust.
Children’s brains are still developing when they are exposed to trauma. At this stage, the brain is still able to expand and mature even if the child is a teenager. Trauma can thwart that growth and affect people in the long run.
At the most basic, biological levels, this damage starts and the trauma alters how the body and brain respond to stress, as well as how the brain produces hormones and neurotransmitters. These modifications affect how the brain develops and are to some extent permanent ultimately causing depression.
4. Stressful Life Events
If you are dealing with an extremely stressful situation in your life, it can cause you to suffer depression. It is crucial to consider the symptoms of depression and get help as soon as possible without delay.
There could be traumatic events in your life that can make you anxious and alone. Many times, people suffering from depression because of a stressful situation in their lives prefer not to share.
But it is essential to understand that talking about a stressful situation to someone reliable can help a lot. Some of the common stressful life events causing depression are:
- Loss of job and long-term unemployment
- Abusive relationship
- Stressful work environment.
- Loss of a loved one
5. Imbalance Of Neurotransmitters In The Brain
Multiple medical disorders can develop when neurotransmitters like dopamine or serotonin levels are abnormal.
Different other conditions that have an impact on various biological processes can also develop from such imbalances. Both neurotransmitters have a great impact on mental health issues including depression.
In fact, dopamine deficiency can even lead to Parkinson’s disease, schizophrenia, and hallucinations along with depression.
Serotonin and noradrenaline, two chemical messengers in your brain that transfer signals between brain cells, are affected by most current antidepressants. For cases of more severe depression, this is assumed to be how drugs function.
In such cases, it is important to seek immediate medical help to bring the situation under control. In order to control mood you can try getting psychological counseling.
New nerve cells can sprout in the circuits that control your mood with an effective treatment. If you are suffering from severe depression, this might help.
6. Certain Types Of Personalities
Some individuals may be more susceptible to depression due to their characteristics and personalities.
For example, it is believed for a good reason that perfectionism is reasonable only to some extent. If you are a perfectionist you may get anxious and stressed if things do not fall into place the way you want them (in a perfect way). This may cause depression in that person due to great dissatisfaction or non-accomplishment.
On the other hand, if you are a person who has extremely low self-esteem, you can also fall for depression after a certain point in your life. Such people often undergo self-doubt, loneliness, sadness, hopelessness, and gradual despair.
7. Chronic Illness
Any chronic illness has the potential to lead to depression, but the risk rises the more serious the condition is and the more disruption it causes in the patient’s life.
The onset of depression triggered by a chronic condition can exacerbate its impact, establishing a detrimental cycle. The likelihood of experiencing depression is heightened when the chronic illness leads to distress, incapacitating symptoms, or feelings of isolation. Subsequently, depression can intensify feelings of pain, fatigue, and self-doubt, potentially causing individuals to withdraw from social situations.
When someone is dealing with a significant, chronic illness, it’s common for people to ignore the signs of depression, thinking that feeling gloomy is normal. It’s crucial to understand what that person’s is actually going through and take a step ahead to help them.
Understanding the brain and its role in depression
The human brain is a remarkable organ that controls every aspect of our thoughts, emotions, and behaviors. When it comes to depression, understanding the intricate workings of the brain is crucial in unraveling its causes. Research has shown that certain regions of the brain, such as the amygdala, hippocampus, and prefrontal cortex, play a significant role in regulating mood and emotions.
Chemical imbalances and depression
One prominent theory regarding the causes of depression revolves around chemical imbalances in the brain. Neurotransmitters, such as serotonin, dopamine, and norepinephrine, are crucial for maintaining proper brain function and mood regulation. When these neurotransmitters become imbalanced, it can lead to depressive symptoms. This theory has paved the way for the development of selective serotonin reuptake inhibitors (SSRIs), a class of medications commonly used to treat depression.
Genetic factors and depression
Depression has been found to have a hereditary component, with studies suggesting that certain genetic variations may increase the risk of developing the condition. While specific genes associated with depression have yet to be identified, researchers believe that a combination of genes and environmental factors contribute to its development. Understanding the genetic factors involved in depression can help in identifying individuals who may be more susceptible to the condition and developing targeted interventions.
Environmental factors and depression
The environment we live in can have a profound impact on our mental health. Adverse childhood experiences, such as abuse, neglect, or trauma, have been linked to an increased risk of depression later in life. Other environmental factors, such as chronic stress, social isolation, and socioeconomic status, can also contribute to the development of depression. By addressing these environmental factors and providing support systems, we can potentially reduce the risk of depression and improve overall mental well-being.
Psychological factors and depression
Our thoughts, beliefs, and coping mechanisms also play a significant role in the development and maintenance of depression. Negative thinking patterns, low self-esteem, and a lack of effective coping strategies can contribute to the onset of depressive symptoms. Cognitive-behavioral therapy (CBT) is a commonly used therapeutic approach that focuses on identifying and challenging negative thoughts and behaviors associated with depression. By addressing these psychological factors, individuals can develop healthier ways of thinking and coping with their emotions.
How do imbalances in brain chemicals contribute to depression?
GABA (Gamma-Aminobutyric Acid) and glutamate are two important neurotransmitters in the brain that play a significant role in mood regulation. Imbalances in these neurotransmitters have been linked to the development of depression.
GABA is an inhibitory neurotransmitter that helps regulate the excitability of neurons in the brain. It helps to calm and relax the brain, promoting a sense of tranquility. When there is an imbalance in GABA levels, it can lead to increased excitability and overstimulation of the brain, which can contribute to symptoms of depression.
On the other hand, glutamate is an excitatory neurotransmitter that is involved in many brain functions, including learning, memory, and mood regulation. Imbalances in glutamate levels can disrupt the delicate balance between excitation and inhibition in the brain, leading to dysregulation of mood and the development of depressive symptoms.
Research has shown that reducing the activity of glutamate and increasing the activity of GABA can have a positive effect on mood and alleviate symptoms of depression. Medications such as selective serotonin reuptake inhibitors (SSRIs) and benzodiazepines are often prescribed to help rebalance these neurotransmitters in individuals with depression. Additionally, therapies such as cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) can also be effective in restoring the balance of GABA and glutamate in the brain.
The link between depression and other medical conditions
Psychological factors, such as personality traits and coping mechanisms, also influence the development of depression. Individuals with low self-esteem, a negative outlook on life, or a tendency to ruminate are more susceptible to depressive symptoms. Additionally, individuals who lack effective coping strategies or have difficulty regulating their emotions may be at a higher risk.
Cognitive-behavioral therapy (CBT) is one approach that focuses on identifying and challenging negative thought patterns and behaviors. By addressing these psychological factors, CBT can help individuals develop healthier coping mechanisms and improve their overall well-being.
How Serious Is Depression?
If you experience one episode of depression, you run the risk of experiencing more in the future. Depression may arise more frequently and become more severe if you don’t receive treatment.
People who are depressed may believe that they may never feel good or happy again. A depressed individual might not appreciate the things they used to love and believe that nothing can make them happy.
For some people with depression, falling asleep at night or sleeping through the night can seem practically impossible. One may face early wake-up and find it difficult to fall back asleep again. Others might snooze for an extended time but still feel exhausted or unrefreshed when they awaken.
As per WHO, an estimated 3.8% of people in the population suffer from depression, including 5.7% of people over 60 and 5% of adults (4% of males and 6% of women). Studies also state that around 280 million people worldwide suffer from depression.
Further, women are around 50% more likely than men to experience depression. Adding to this, more than 10% of pregnant and recently delivered women experience depression globally.
Relationships can adversely suffer when you go under depression. One may find it difficult to focus on work which can also affect health, and in certain circumstances, it might even result in suicide.
When depressed, there is a higher risk of suicide. About 60% of those who die by suicide, according to researchers, have a mood problem such as depression or bipolar disorder. In reality, depression is a factor in close to 40,000 suicides in the US annually. Not only adults but teenagers, and children are also susceptible to committing suicide.
It is also found that teenagers and young adults who commit suicide frequently struggle with substance abuse and depression. When someone doesn’t receive the necessary support, those difficulties frequently worsen.
Even though there are proven, effective treatments for mental illnesses, more than 75% of people in low-and middle-income countries do not receive therapy. The provision of quality care is hampered by a lack of financing for mental health services and a staffing deficit.
How Can Depression Trigger Suicide?
A person with depression frequently has different thinking. A chemical imbalance may be to blame for this, which may make it difficult for the sufferer to know what solutions are open to them to end their suffering.
Many depressed individuals claim to feel as though they are unable to envision a bright future or recall a joyful past. Asking for help might not even cross their minds because they are not in a state to realize that they have a disease that can be treated. Even physical pain and emotions can become intolerable.
They feel that death is their only hope of ending their suffering, even though they don’t want to die. It’s a genuinely crazy decision! Like having cancer or diabetes, suffering from depression is an involuntary condition that can be diagnosed, treated, and managed.
Treating depression: Medications and therapy options
Depression is a complex illness with a multitude of factors contributing to its development. One significant factor is the imbalance of brain chemicals, also known as neurotransmitters. Neurotransmitters are chemical messengers that facilitate communication between neurons in the brain.
Serotonin, dopamine, and norepinephrine are three neurotransmitters that have been extensively studied in relation to depression. Imbalances in these neurotransmitters can disrupt the intricate network of brain circuits involved in mood regulation, leading to the onset of depressive symptoms.
Serotonin is also known as the neurotransmitter that makes us feel good. It regulates mood, sleep, appetite, and overall well-being. Low levels of serotonin have been associated with depression, as they can lead to feelings of sadness, irritability, and a loss of interest in activities that were once pleasurable.
In contrast, dopamine is linked to motivation, reward, and pleasure. It plays a crucial role in the brain’s reward system, which is responsible for reinforcing behaviors that are essential for survival. Imbalances in dopamine can result in a lack of motivation, anhedonia (the inability to experience pleasure), and a general feeling of apathy.
Noradrenaline or norepinephrine is a neurotransmitter that plays a role in the body’s stress response. It helps to regulate attention, alertness, and arousal. Imbalances in norepinephrine can lead to symptoms such as fatigue, difficulty concentrating, and a sense of hopelessness.
While imbalances in these neurotransmitters are not the sole cause of depression, they are believed to play a significant role in its development. Medications such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed to help rebalance these neurotransmitters and alleviate symptoms of depression. However, it is important to note that each individual’s brain chemistry is unique, and what works for one person may not work for another. This is why finding the right treatment approach often requires a trial-and-error process.
Lifestyle changes to support mental health and balance brain chemistry
When it comes to treating depression, there is no one-size-fits-all approach. The most effective treatment plan often involves a combination of medications and therapy options tailored to each individual’s needs.
Medications like antidepressants are usually given to help balance out the chemicals in your brain and reduce the symptoms of depression. SSRIs (Selective Serotonin Reuptake Inhibitors) are widely prescribed antidepressants. They work by increasing the levels of serotonin in the brain, which helps regulate mood and alleviate depressive symptoms. Other types of antidepressants, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs), target multiple neurotransmitters to provide relief from depression.
In addition to medications, therapy options are an essential component of treating depression. Cognitive-behavioral therapy (CBT) is one of the most effective forms of therapy for depression. It focuses on identifying and changing negative thought patterns and behaviors that contribute to depressive symptoms. CBT helps individuals develop coping strategies and problem-solving skills to better manage their emotions and improve their overall well-being.
Other therapy options for depression include interpersonal therapy (IPT), which focuses on improving relationships and resolving interpersonal conflicts, and psychodynamic therapy, which explores the unconscious processes that contribute to depression. Additionally, alternative therapies such as mindfulness-based stress reduction (MBSR), art therapy, and exercise therapy have also shown promising results in improving mood and reducing depressive symptoms.
It is important to note that finding the right treatment approach may take time and patience. Not all medications or therapy options work for everyone, and it may be necessary to try different approaches or combinations to find what works best for each individual. Working closely with a healthcare professional is crucial in developing an effective treatment plan and ensuring the best possible outcome.
How Can We Help You?
We at Relevance Recovery deliver thorough and efficient care that takes into account the complicated and delicate nature of mental health and substance use problems. We aim to work to improve people’s quality of life and aid in sustained rehabilitation.
As your committed partner on the road to mental health and well-being, we are here for you! We provide priceless tools and insights for tackling substance misuse and managing mental health issues like depression.
Our program is constantly evolving as a connected community of Medical and Clinical professionals, including fresh research and evidence-based techniques. Each participant in our program receives a unique treatment plan using a variety of therapeutic modalities.
The treatment program takes into account the demands of the person’s emotional, mental, physical, and spiritual well-being. We consistently try to identify and address structural barriers that impede marginalized people from getting care because we believe that everyone should have access to high-quality healthcare.
We also offer successful relapse prevention techniques through our acclaimed programs, assuring a long-lasting and transformative recovery journey. Come with us as you embark on your healing process to lead a happier, and healthier life.
Reach out to us at our Holistic Depression Treatment Centre in New Jersey by filling out a form here to request a callback.
The Final Say
Depression is a serious, chronic medical condition that can affect every aspect of a person’s life. It often leads to suicidal thoughts which can be very serious and fatal.
This isn’t something you can just get over with a good night’s sleep. You can treat it and improve your chances of healing by getting help.
It is crucial for a patient to consult a doctor with experience in treating depression and to be open to trying a variety of treatments because depression can be difficult to treat. Therapy and medicine often go hand in hand to get the best results.









