Have you ever felt like your mind is constantly at war with itself, racing one day, barely moving the next? Like your energy surges at 2 a.m., but when the world expects you to function, you’re paralyzed by exhaustion or despair? If this feels painfully familiar, you’re not alone, and more importantly, you’re not broken.
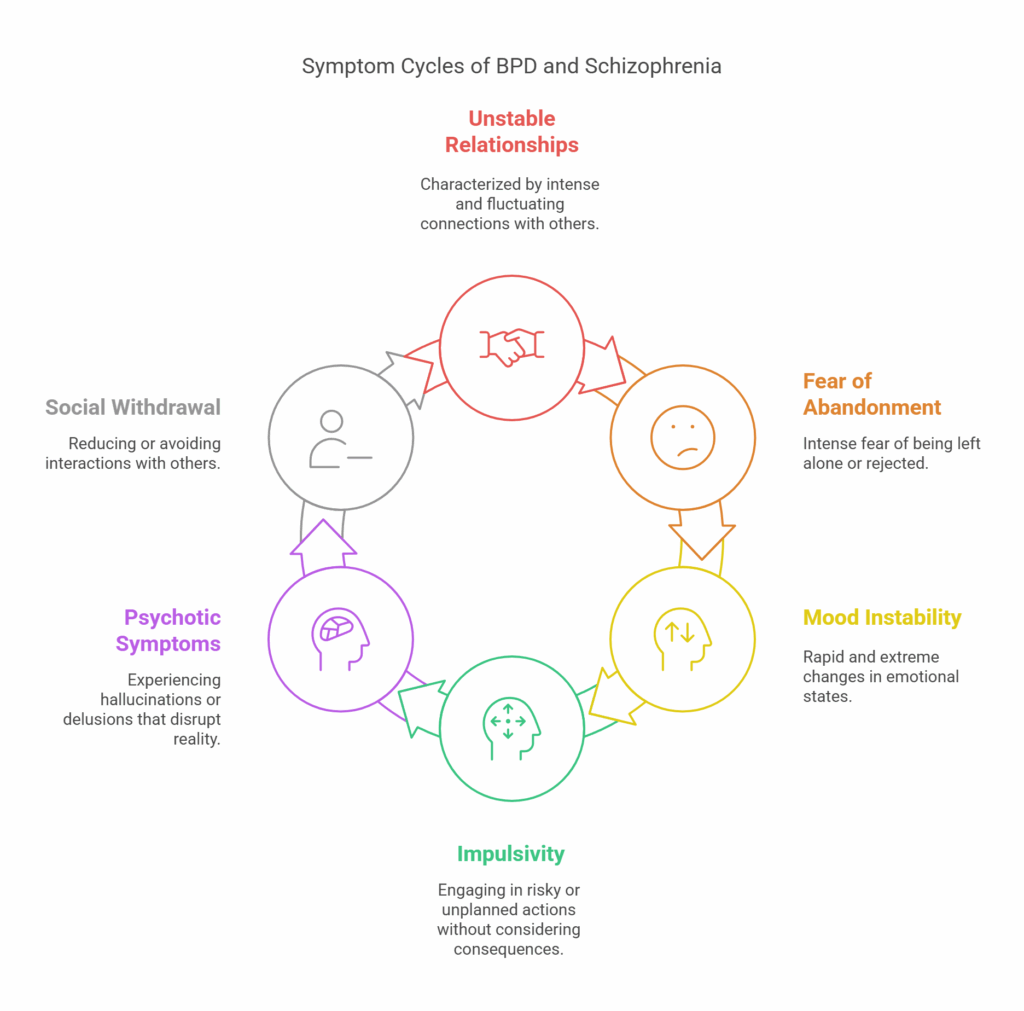
Bipolar disorder isn’t just a label. It’s the invisible chaos behind smiling photos, unfinished projects, broken routines, and strained relationships. It’s the unpredictable shift from feeling invincible to feeling invisible. And for so many people, it’s not just difficult,it’s devastating.
But here’s what most people don’t talk about: there is help. There is hope. And there are treatment paths that actually work.
At Relevance Recovery, we believe that understanding the most effective treatment for bipolar disorder is the first step toward taking back control. Whether you’re seeking answers for yourself or someone you love, this guide will walk you through the real-life options that bring real-life change ,because healing isn’t just possible. It’s waiting.
Understanding Bipolar Disorder
Bipolar disorder is a mental health condition characterized by significant mood swings, including episodes of mania and depression. These episodes can impact sleep, energy levels, behavior, judgment, and the ability to think clearly. Approximately 4.4% of U.S. adults experience bipolar disorder at some point in their lives.
The disorder is typically classified into three types:
- Bipolar I Disorder: Defined by manic episodes lasting at least seven days or by manic symptoms severe enough to require immediate hospital care. Depressive episodes also occur, typically lasting at least two weeks.
- Bipolar II Disorder: Characterized by a pattern of depressive episodes and hypomanic episodes, which are less severe than full-blown manic episodes.
- Cyclothymic Disorder (Cyclothymia): Involves periods of hypomanic symptoms as well as periods of depressive symptoms lasting for at least two years (one year in children and adolescents); however, the symptoms do not meet the diagnostic requirements for a hypomanic episode and a depressive episode.
Effective management of bipolar disorder requires a comprehensive approach tailored to the individual’s specific symptoms and needs.
Comprehensive Treatment Approaches at Relevance Recovery
At Relevance Recovery, we recognize that the most effective treatment for bipolar disorder involves a multifaceted approach. Our treatment programs are designed to address the unique needs of each individual, integrating various therapeutic modalities to promote lasting recovery.
Pharmacological Interventions
Medication often plays a pivotal role in stabilizing mood fluctuations associated with bipolar disorder. Our medical team works closely with clients to determine the most effective medication regimen, which may include:
- Mood Stabilizers: Medications such as lithium and valproate are commonly used to control mood swings and prevent relapse.
- Antipsychotic Medications: Second-generation antipsychotics like quetiapine and olanzapine can be effective, particularly during manic episodes. Quetiapine is effective for all phases of bipolar disorder, acute mania, acute depression, and maintenance therapy.
- Antidepressant Medications: These are used cautiously and typically in combination with mood stabilizers to mitigate the risk of triggering manic episodes.
It’s important to note that medication management is highly individualized, and our team continually monitors and adjusts treatment plans to ensure optimal outcomes.
Psychotherapeutic Interventions
In conjunction with medication, psychotherapy provides individuals with strategies to manage symptoms and improve coping mechanisms. At Relevance Recovery, we offer a range of therapeutic modalities, including:
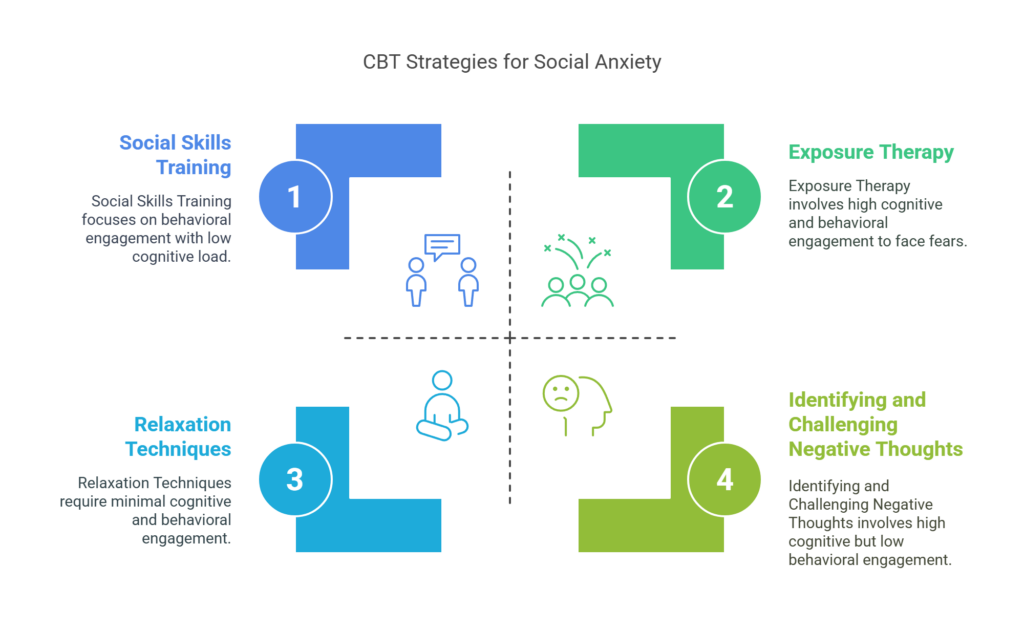
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns and behaviors.
- Dialectical Behavior Therapy (DBT): Emphasizes mindfulness, emotion regulation, and interpersonal effectiveness.
- Family Therapy: Involves family members in the treatment process to improve communication and support.
- Group Therapy: Provides a supportive environment where individuals can share experiences and coping strategies.
These therapies aim to equip individuals with the tools necessary to navigate the challenges of bipolar disorder effectively.
Holistic and Lifestyle Interventions
Recognizing the importance of holistic well-being, Relevance Recovery incorporates lifestyle interventions into our treatment programs:
- Nutritional Counseling: Guidance on balanced diets to support overall health and mood stability.
- Exercise Programs: Regular physical activity can have a positive impact on mood and energy levels.
- Mindfulness and Stress Reduction Techniques: Practices such as yoga and meditation to promote relaxation and emotional balance.
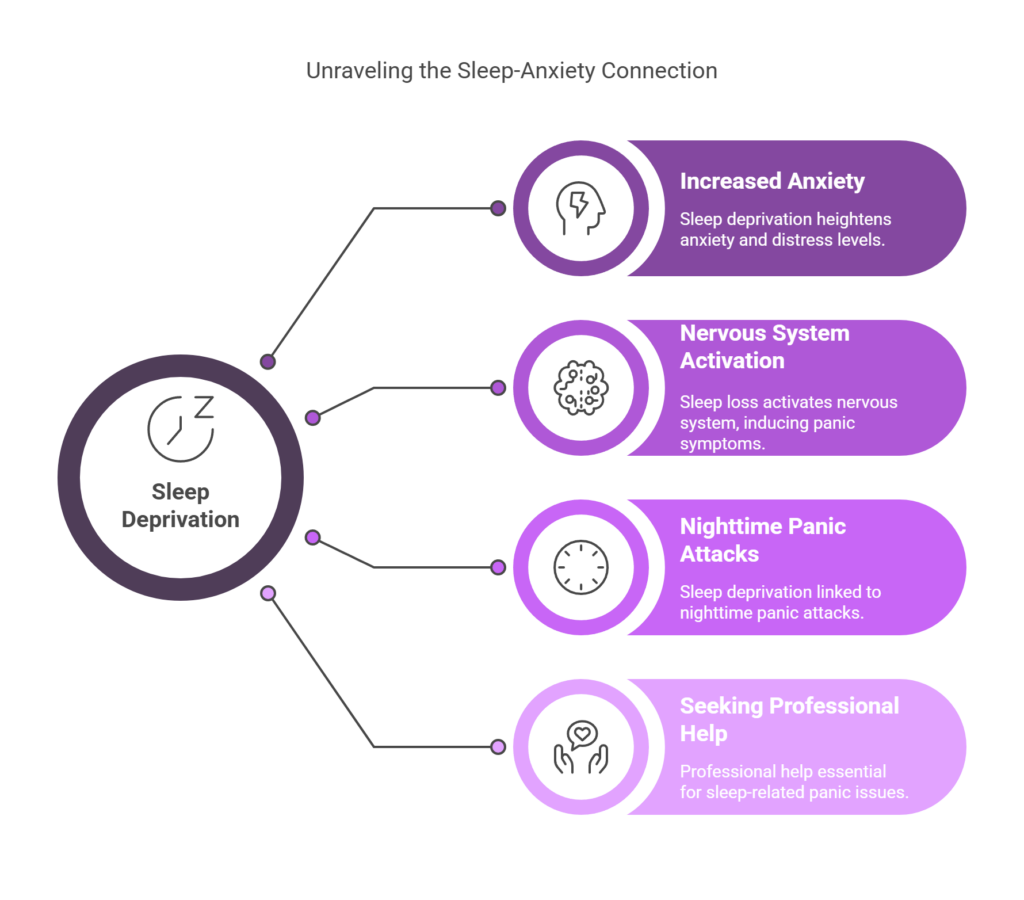
- Sleep Hygiene Education: Strategies to establish consistent sleep patterns, which are crucial for mood regulation.
By addressing these lifestyle factors, we aim to enhance the overall effectiveness of treatment and support long-term recovery.
Specialized Programs and Support Services
Relevance Recovery offers specialized programs tailored to meet the diverse needs of our clients:
- Adolescent Mental Health Programs: Focused support for teenagers navigating bipolar disorder, incorporating age-appropriate therapies and family involvement.
- Supportive Housing: Safe and structured living environments to aid in the transition from treatment to independent living.
- Aftercare and Alumni Programs: Ongoing support to maintain recovery gains and prevent relapse.
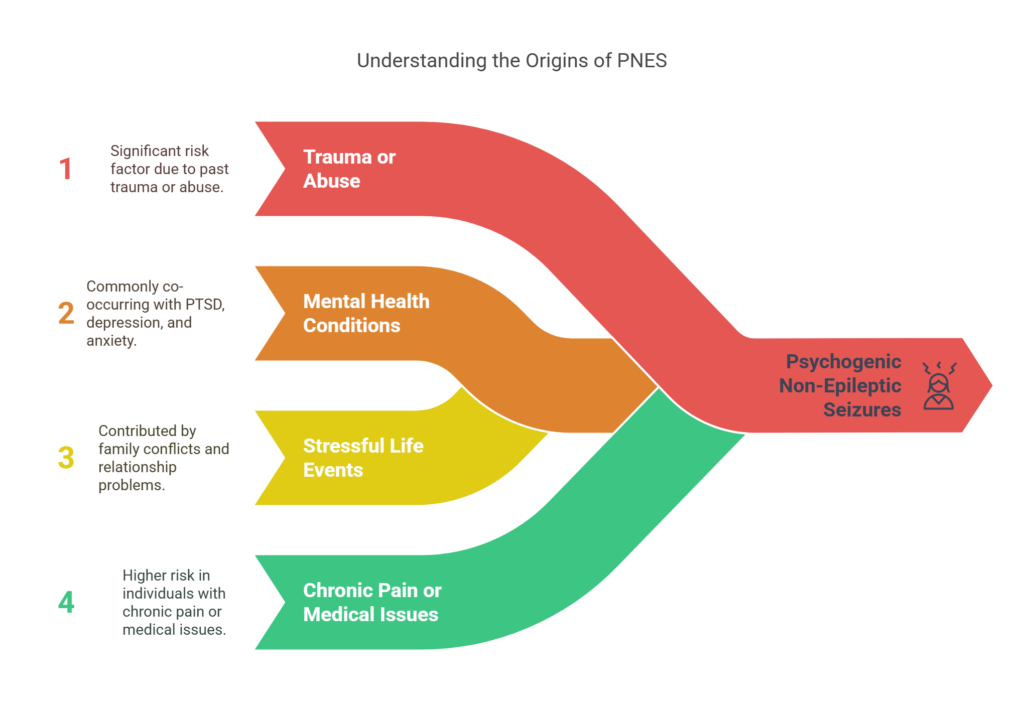
- Dual Diagnosis Treatment: Integrated care for individuals experiencing co-occurring substance use disorders and bipolar disorder.
Our comprehensive services ensure that individuals receive the support they need at every stage of their recovery journey.
Innovative Therapies and Research
Staying at the forefront of mental health treatment, Relevance Recovery incorporates innovative therapies and remains engaged with current research:
- Esketamine Treatment: An option for treatment-resistant depression associated with bipolar disorder.
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, which may improve symptoms of depression.
- Ongoing Research Participation: Our commitment to evidence-based practices involves staying updated with the latest studies and integrating new findings into our treatment approaches.
By embracing these advancements, we strive to provide our clients with the most effective and cutting-edge treatments available.
There is help. There is healing. And there is a way forward.
If you’ve made it this far, chances are you’re not just skimming through options, you’re searching for a real answer. Maybe you’re exhausted from the ups and downs, or maybe you’re watching someone you love disappear into a cycle of moods you can’t control. It’s okay to admit that this is hard because it is.
But here’s the truth: bipolar disorder doesn’t get to write the final chapter of your story.
Finding the most effective treatment for bipolar disorder isn’t about chasing a miracle cure, and it’s about building a plan that meets your specific needs. Whether it’s medication, therapy, lifestyle changes, or a combination of all three, what matters most is that your treatment works for you. And the best outcomes happen when you’re supported, understood, and empowered.
At Relevance Recovery, we’re here to help you do just that. With evidence-based therapies, compassionate professionals, and a deep respect for your journey, we walk with you, with no judgment or pressure, just the path to something better.
If you or a loved one is seeking the most effective treatment for bipolar disorder, now is the time to take that first step because you’re not alone. And you never have to face this alone again.
FAQs
1. What is the most effective treatment for bipolar disorder?
The most effective treatment for bipolar disorder combines medication and therapy. Mood stabilizers like lithium or antipsychotics help manage highs and lows, while therapy offers emotional support and teaches healthy coping skills. A personalized plan from a professional treatment center improves long-term stability and well-being.
2. Can bipolar disorder be treated without medication?
Some people benefit from therapy and lifestyle changes alone, but most need medication to control severe mood swings. Without medication, symptoms can return quickly. It’s important to speak with a mental health provider to find a safe, balanced approach that works for your specific needs.
3. How long does treatment for bipolar disorder take?
Bipolar disorder is a lifelong condition, so treatment is ongoing. While symptoms can improve over time, long-term support helps prevent relapse. Consistent medication, therapy, and monitoring are key. Many individuals manage symptoms well and lead full lives with professional guidance and a strong treatment routine.
4. What kind of therapy helps with bipolar disorder?
Therapies like Cognitive Behavioral Therapy (CBT), psychoeducation, and family-focused therapy are helpful. These therapies teach people to manage stress, recognize early warning signs, and communicate better with loved ones. Therapy works best when combined with medication and a supportive, structured environment like Relevance Recovery offers.
5. How do I know if my treatment is working?
You’ll notice fewer mood swings, better sleep, improved focus, and stronger relationships. Progress might be slow, but consistency matters. Keeping a symptom journal and staying in touch with your treatment team helps track improvement and adjust the plan as needed for the best results.
6. Can lifestyle changes really make a difference in treatment?
Yes! Daily routines, healthy eating, regular sleep, and exercise help support brain function and reduce stress. Avoiding drugs or alcohol is also crucial. These habits don’t replace medication but enhance its effects. A structured lifestyle supports emotional balance and strengthens treatment outcomes over time.
7. Is there a cure for bipolar disorder?
There’s no cure for bipolar disorder, but it can be managed successfully with proper care. With medication, therapy, and strong support, symptoms can be controlled. Many people live fulfilling lives by working closely with professionals and following a consistent treatment plan tailored to their needs.
8. What happens if bipolar disorder is not treated?
Without treatment, bipolar disorder can lead to severe mood episodes, risky behavior, job or relationship loss, and even hospitalization. It may also increase the risk of substance abuse or suicide. Seeking help early provides a better chance for recovery and long-term emotional stability.
9. Can someone with bipolar disorder live a normal life?
Absolutely. With the right support system, consistent treatment, and healthy routines, people with bipolar disorder can have successful careers, relationships, and goals. Treatment makes symptoms manageable, allowing individuals to regain control of their lives and find stability in the middle of emotional ups and downs.
10. How can Relevance Recovery help someone with bipolar disorder?
Relevance Recovery provides comprehensive treatment plans for bipolar disorder that include therapy, medication management, and ongoing support. Our compassionate team understands each person’s unique journey and offers care that’s personalized, nonjudgmental, and empowering, helping clients manage bipolar disorder and build a healthier, more stable future.